Trabeculectomy
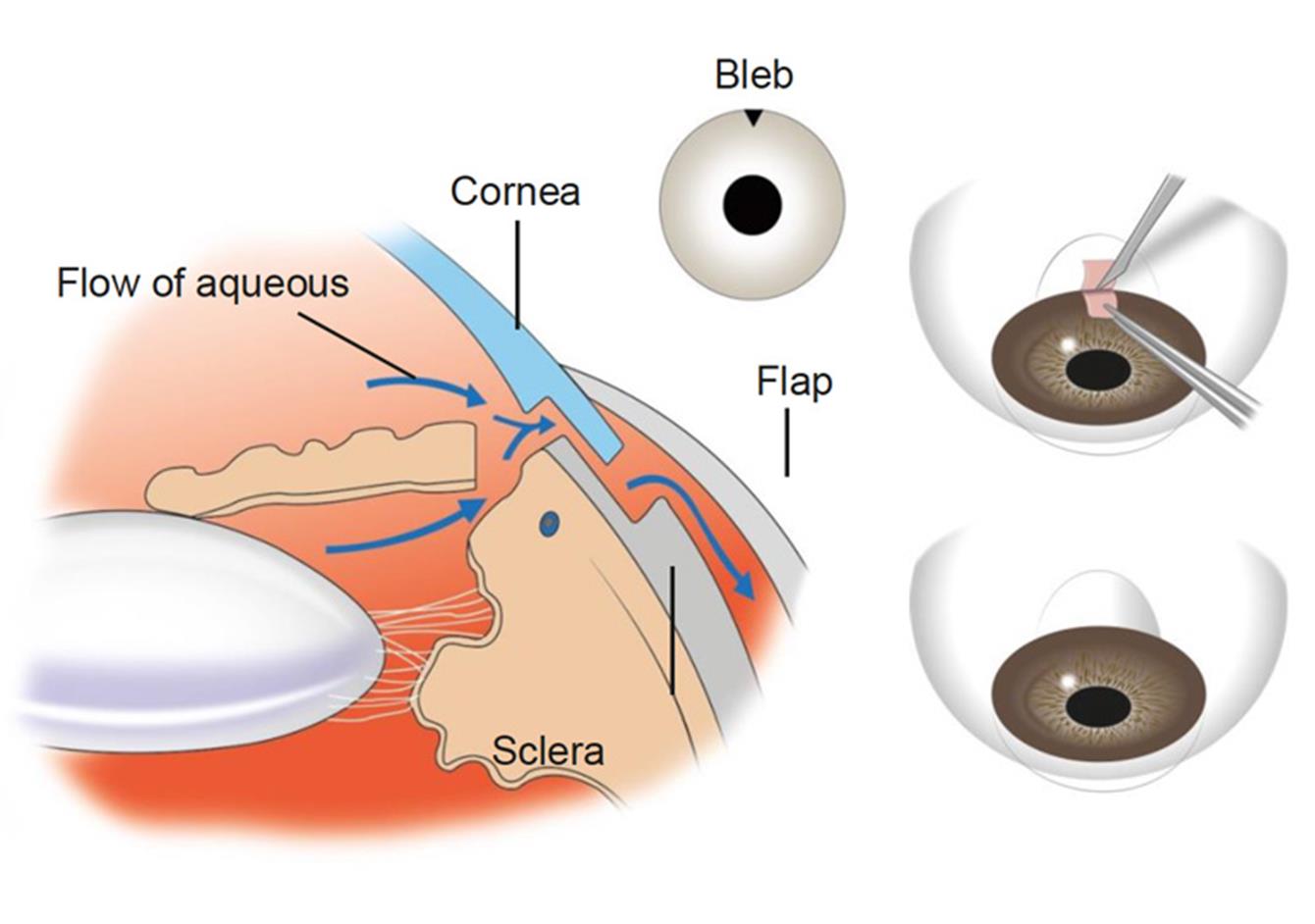
Diagram showing flow of fluid through normal trabeculectomy and position of bleb on the eye.
A trabeculectomy is a surgical operation for patients with glaucoma.
The procedure involves making a safety valve/ ‘trap door’ in the sclera of the eye (white part) underneath the upper lid. This allows some of the fluid inside the eye to drain out via a different route. The goal of the surgery is to optimise the pressure inside the eye, keeping it at a safe level and preventing further damage to the optic nerve and visual field.
A trabeculectomy will not restore vision that is lost due to glaucoma.
In general, it is more than 80% successful at reducing eye pressure and keeping it under control. It may still be necessary for you to continue eye drops after surgery.
The procedure typically takes 50 to 80 minutes (IGA, 2015) and is done under either local or general anaesthetic. The procedure is usually done as a day case procedure. We also consider what support you have at home.
Eye appearance
There will be a little blister (bleb) on the upper part of the eyeball, which is under the eyelid, and it is not usually noticeable. This is where the ‘trap door’ is made to allow fluid to drain from inside of your eye to the space under the fine layer covering the eyeball (conjunctiva).
Alongside this, you may notice some redness and swelling of the eye and lids. Immediately following the surgery, you will have a patch on the eye and you should wear this at night to protect the eye while you sleep.
Blurring of vision
You may find that your vision is blurred for several weeks after the operation, until the operation site is healed. The operation will not restore any sight you have already lost, it is to save the sight you have.
Discomfort in the eye
Mild pain and discomfort are common in the post-operative period, this is partly due to the surgery itself, and partly due to the stitches. Some of the stitches do not dissolve and may be removed in clinic 2-3 weeks after surgery- this takes 2-3 minutes with anaesthetic eye drops. Eyes usually start to feel more comfortable in around two weeks’ time.
It is important to continue any eye drops to the UNOPERATED eye unless Mr Agarwal tells you otherwise. Do not use your usual glaucoma drops in the operated eye after the operation unless Mr Agarwal tells you.
It is very important to keep to the prescribed treatment of drops following a trabeculectomy surgery. This is one of the key components in the long term success of the operation.
The eye will remain numb throughout the surgery. If you are aware of any pain, please let Mr Agarwal know, as this is unusual. The initial numbing of the eye is done with a drop followed by an injection. You may be aware of slight discomfort and pressure as the anaesthetic is delivered.
Throughout the surgery you may see bright lights and hear people talking. Only your eye will be visible to Mr Agarwal, the remainder of your face will be covered with a sterile drape to keep the operation sterile.
Often, at the end of the surgery a special drug is used to help prevent scarring of the passage for the fluid. This is called mitomycin C (MMC) and is a type of anticancer drug. This is applied to only a certain part of the surgical site. This drug has been used for many years in eye surgery and has been found to be safe; however, is not what it was originally licensed for and it’s use if termed ‘off license’.
Infections
If you get a red or sticky eye with discharge please get in touch without hesitation, it’s important to be seen as soon as possible. As the trabeculectomy has made a passage way into the eye, it is possible to get an infection inside the eye called endophthalmitis which can be sight threatening. Early treatments of any infections can help to avoid this complication.
Stiches
Loose stiches can be an irritation for you and can cause the eye to become red, sore and possibly inflamed or infected. These will need to be removed and this can usually be done in the clinic.
Cataract
A long-term side effect of any surgery done to the eye is the quickened development of a cataract in this eye. When this happens a surgery to remove it can be arranged.
Pressure
There is the possibility after surgery of the pressure in the eye becoming too low or too high. This may require further surgery or modification of drops. Mr Agarwal will talk to you about your individual circumstances.
Difference between eyes
You may be aware after the surgery that your pupil or even the eyeball are a different shape when compared to your other eye. This typically doesn’t affect your vision and is a result of the surgery. Typically you will not be aware of able to see the bleb that was formed during surgery.
Do…
- Wear your glasses throughout the day as normal, if you have them.
- Continue to read and watch TV.
- Wear sunglasses to reduce light sensitivity, if needed.
- Wash you hands before inserting drops.
- Wear an eye shield at night for as long as recommended by Mr Agarwal.
- Keep to a routine with drop insertion. If you have a smart phone, there are apps you can download to help you with this or many patients make a chart.
- Arrange to take some time off work if you’re working, this can depend on the individual and type of work required.
- Ask any questions you may have.
Don’t…
- Wear contact lenses until cleared by Mr Agarwal.
- Wear eye make-up for at least 2 weeks ideally 4 weeks following surgery.
- Touch the tip of the eye drop bottle with your fingers or to your eye.
- Bend over, stain or undertake strenuous activities like weight lifting running, biking or inversions in yoga.
- Put pressure on your eye for at least four weeks, this will aid in the healing process.
- Update your glasses within the first 3 months of surgery.
- Be afraid to ask questions.
Further Information
Accuracy
While care has been taken to compile accurate information and to keep it up to date, Mr Agarwal cannot guarantee its correctness and completeness. The information provided in this information sheet is designed to support care and is not a substitute for professional healthcare advice, by a qualified doctor or other healthcare professional, which will be tailored to a patient’s individual circumstances.
